The Hemp Connection [Search results for nervous system]
Omega-3's are great for mental health--and >80% of women with PCOS are struggling with mental health issues

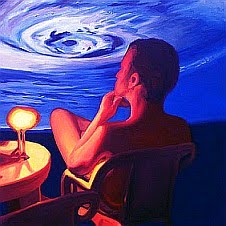
Which came first, the stress or the racing thoughts?

It might start sooner than you think!
Ways to keep from losing your mind

If only I had bet my money on whether Meridia would find itself in trouble…

Revisiting chia

If you have PCOS and exercise is truly a PAIN, take note, there may be an explanation as well as a solution

When the Mahareshi Mahesh Yogi Hit “The Big Tomato”

What does it mean to have an inflammatory disease?

How Much Carbohydrate is the Right Amount of Carbohydrate?

Are you depressed because of your weight? Or are you depressed because you're depressed?

Psychiatric/nervous system medications may be affecting your PCOS, and carnitine may help

Today I am contemplating…PCOS. Or a much bigger picture?
Now hear this! If you're pregnant, you absolutely, positively, need to be fish-friendly

A note to physicians prescribing metformin to women with PCOS

Who cares how well you eat and how much you move? If you're not respecting sleep, you've got a huge health risk

Nutrition may be one of the most important weapons against secondary infertility

At inCYST, it's not just about getting pregnant, we aim to create healthy adults from the moment they are conceived!

Fat, lazy, and stupid…or hormone-imbalanced, exhausted, and brain fogged?

Is it an eating disorder…or is it PCOS?